Healthy hydration practices and obesity:
Healthy hydration practices and obesity: What do you drink?

Healthy hydration practices and obesity. the question to ask is what do you drink and does it add value to your life?
Looking at the ever increasing prevalence of different health conditions like overweight, obesity, type 2 diabetes and other weight related conditions across the globe, one would be forgiven to wonder what the matter is really. In spite of the numerous efforts made by various institutions based the guidance from the experts like clinicians, innovative campaigns targeting the general public and widespread government public health initiatives, yet still little is being achieved. In view of this, it is obvious that a time has come for the application of a different approach. Could it be that we are missing or just ignoring something very important? Experts at AWAREmed Health and Wellness Resource Center led by the founder of the facility Doctor Dalal Akoury has been evaluating options. It then became clear that many people are not just keen on healthy hydration practices and obesity implications.
In respect of this we came to realize that the importance of fluid intake and particularly water has been overlooked in campaigns and guidelines and also in the clinical setting, where the question ‘what do you drink?’ has been a constant omission. This is a significant oversight that food pyramids and healthy-eating plates across the world omit fluids from their graphics and advice. While guidelines include recommendations on changes in physical activity and diet, often little or no advice is offered on the importance of healthier hydration practices, ignoring to highlight the contribution of beverages high in sugar, alcohol or additives is one terrible mistake we often make.
Healthy hydration practices and obesity: Is it true that water is life?
It is believed that of all the body organs, the brain is one of the most critical of all. This is so because it controls every other functions of the body. Like for instance when you talk of energy, the brain uses water and food. Water feeds the brain’s hydro-electrical needs and food contains sugar (or its derivatives), which the brain uses for functioning. Doctor Akoury introduces something very interesting that subject to certain situations, the body can go for months without food yet it can only live for a few difficult weeks without water. What does this communicates to you? It simply means that food is a less important energy source in relation to water. In other words when the brain and body run low on energy, we’re not hungry but are thirsty. It is very important that every one of us should pay attention to health hydration and obesity if we are to remain in good health.
Either food or water will be deposited into the stomach, so it produces acid to signal the energy requirement. Unfortunately, we call this alert “hunger pangs” and usually satisfy them by eating. This quiets the stomach momentarily. But there’s still no water input, so the pangs return and we eat again. Still, there is no water for the brain (let alone for the rest of the body). This causes more pangs so we eat again and the consequences of overeating are well known to us. Nonetheless when the stomach becomes full, it stretches, and that tells the brain it has had enough food for now. However when we continue to eat, the brain ignores the stretch signal to stop, thus removing the natural mechanism to prevent excessive food intake. By ignoring the stretch signal to stop, we eat again and again expecting an energy boost. Instead we become obese.
The food that we eat has to be digested and takes a while to become useful, and the excess is stored as fat. Food might be considered a “dirty fuel” because it uses up valuable energy and water in digestion and most of the energy value is stored as body fat. Remember that stuffing your stomach with more food before the previous food has been fully digested may lead to indigestion, gas and bloating. Two glasses of water will have more effect than any antacid or gas-reducing medication by diluting the stomach acid that causes those symptoms. That is why healthy hydration practices and obesity awareness is the way to go because water is clean energy because any excesses or that which may be considered as impurities are passed out through the kidneys as urine, does not need the digestive process, and goes to work immediately.
A glass of water before meals stimulates the sympathetic system to activate lipase to break down fat for energy use. For up to two hours this water also stimulates the intestines to release motilin which informs the brain that water is available; thus quieting the stomach’s “hunger pang” cries for water. This hormone also acts as a laxative, so that with water’s lubricating effects, causes easy bowel movements.
When you give water a chance to fulfill its primary role in energy supply, the natural desire for food will shift from starch to protein and fat, so the craving for sweets will diminish.
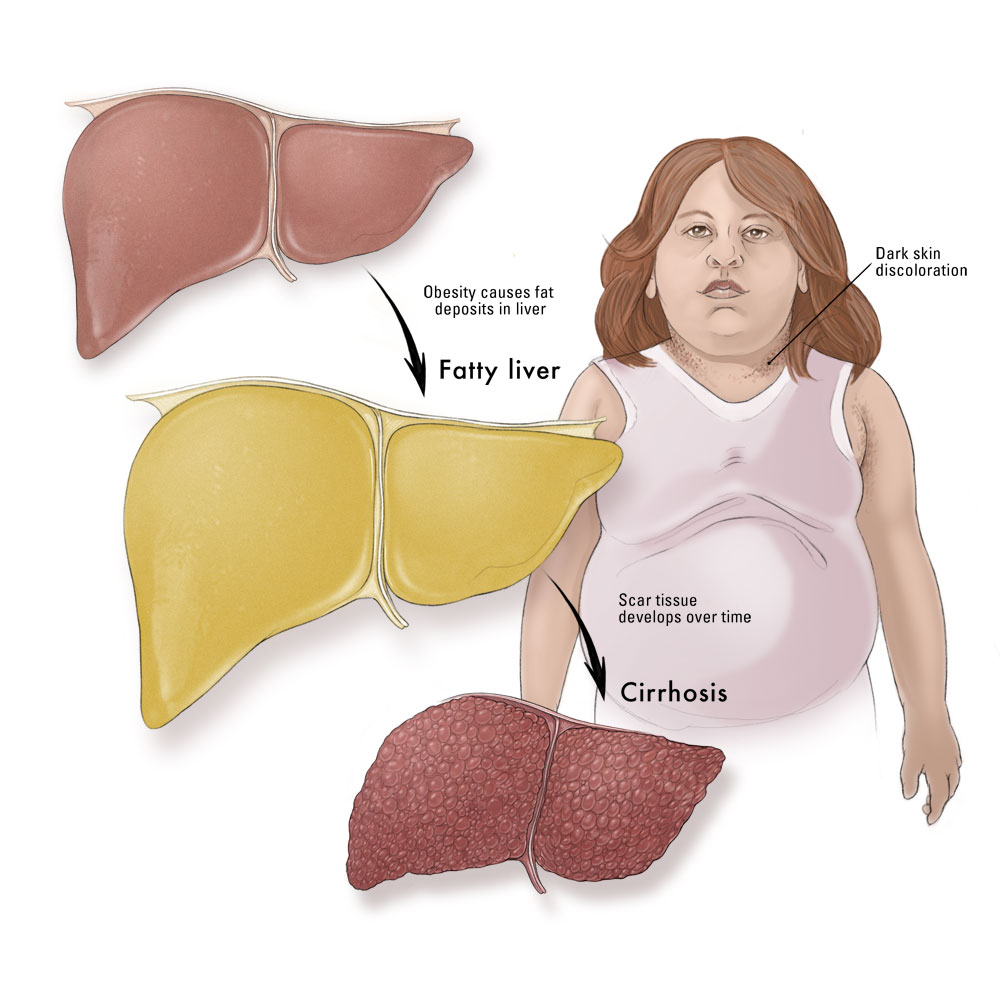
If the over-eating and lack of water continue however, the resulting obesity can lead to diabetes. The experts recommends that people should drink water which is equivalent to one half their body weights. It should be noted that this recommendation is to keep us from getting dehydrated. Re-hydrating that same body will require more than ten glasses per day. When salt is also taken during re-hydration, it helps balance the blood sugar levels and reduces the need for insulin injection.
The experts are also explaining why dehydration is detrimental for the diabetic. Drinking gives “the pancreas the fluid it needs to properly produce the insulin that regulates blood sugar levels. In fact the metabolism of sugar is a very fluid-dependent system that quickly suffers if fluid intake is in any way limited.” Fluids require digestion and are not as effective as water. Coffee and tea are diuretics and thus wash out any water contained in them. Only water itself effectively combats dehydration and the need for water.
Healthy hydration practices and obesity: Type II diabetes
When the pancreas does not receive the water it needs, Type II diabetes results when prostaglandin-E 2 inhibits insulin release no matter how much of it is available. The body may also coat the insulin molecules with xanthurenic acid so the insulin receptors no longer recognize it.
When blood glucose levels are higher than they should be for prolonged periods of time, the kidneys remove some of the excess glucose from the blood and deposit it in the urine. Since some water is required to produce that urine, the dehydrated body may steal it from eye tears, saliva, and water stored in body cells. This is why diabetics experience frequent urination, increased thirst, dry mouth and eyes. It is generally accepted that diabetes runs in families and is a genetic problem. It is said you can’t prevent diabetes (unless you stay slim) and may eventually have to cope with the disease. Dr. Akoury maintains that dehydration does indeed mutate our genes.
It could also be noted that our parents teach us how to take care of ourselves. “Eat. Brush your teeth. Be careful crossing streets.” How often were you told, “Drink your water”? Perhaps as children, we don’t learn from our parents how to stay hydrated to prevent obesity and diabetes. And our parents didn’t learn to drink water from their parents; ergo dehydration and its effects runs in families. Finally if this was not done for you, then be the one to bring in the difference. Show your children the best and healthy hydration and obesity preventions today. If you are having any concern to raise with the experts, then you can schedule for an appointment with doctor Akoury today.
Healthy hydration practices and obesity: What do you drink?