Motherhood obesity and overweight

Motherhood obesity and overweight affects most young women today
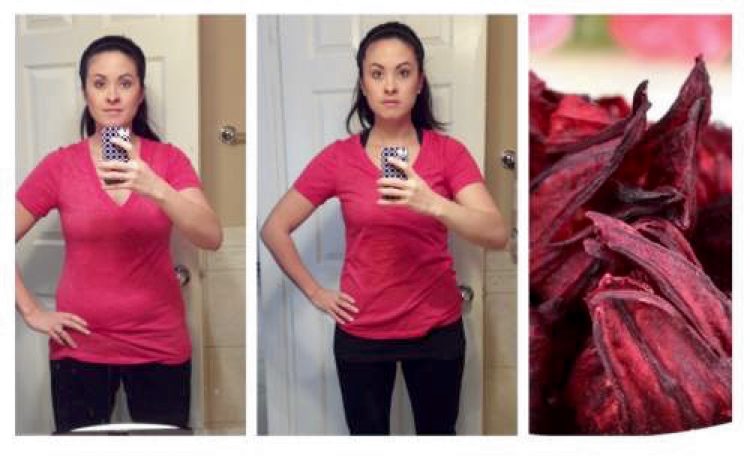
Motherhood obesity and overweight: Emotional worries of pregnant women
Life has a lot to offer in a family setup. Each family member will be pulling together to contribute positively to the well-being of the family unit. While we appreciate the efforts made by each member, there are certain times when mothers find themselves playing double roles in the family. These are the times when each member of the family is physical, emotionally, economically and spiritually getting ready to receiving a new member of the family. When everyone is waiting, mothers who bear the greatest burden go through experiences that no one can contemplate narrating if you are not a mother. I am talking about the emotional worries of our mothers when nursing pregnancy. With all these, you can only imagine if one is also obese. And that is why we want to discuss matters concerning motherhood obesity and overweight.
Some of the worries of obese expectant women can trigger depression a condition which is not good for anyone’s health. What do these ladies go through in this state of pregnancy? Certainly, these ladies have many questions. We sought expert’s opinion from doctor Dalal Akoury MD President and founder of AWAREmed health and wellness resource center and she are responding to some of their concerns as we progress in this article.
Motherhood obesity and overweight: Will I need specialized care during pregnancy?
All pregnant women will certainly be attended to regularly by their healthcare providers however if you are obese and pregnant, your health care provider will make a close observation on you and depending on your condition they may make the following recommendations:
Early testing for gestational diabetes – if in the opinion of your doctor you stand a greater risk of gestational diabetes he may order a screening test called the glucose challenge. This test is done between 24 and 28 weeks of pregnancy, nonetheless, the doctor may recommend this test a little bit earlier in your pregnancy sometimes even at your first prenatal visit and if your test results are normal, you’ll likely repeat the same screening test between 24 and 28 weeks of pregnancy. It must be noted that these recommendations by the doctor will be applicable for only pregnant obese women.
Delayed fetal ultrasound – the emergence of technology has introduced fetal ultrasound a technique that uses high-frequency sound waves to produce images of the baby in the uterus. Fetal ultrasound is conducted between week 18 and 20 of pregnancy to assess the baby’s growth and development. Because this technology uses ultrasound waves don’t easily penetrate abdominal fat tissue, being obese during pregnancy will mean that there will be lots of fat tissues around the abdomen which will create interference or hindrance with the effectiveness of fetal ultrasound meaning that ultrasound results might be more detailed if the test is done a few weeks later, say between weeks 20 and 22 of pregnancy.
Fetal echocardiography – your health care provider might recommend a fetal ultrasound that provides a detailed picture of your baby’s heart (fetal echocardiography) between weeks 20 and 22 of pregnancy. This test is used to rule out or confirm a congenital heart defect.
Frequent prenatal visits – as your pregnancy progresses, your health care provider might recommend more frequent prenatal visits to monitor your health and your baby’s health. Regular fetal ultrasounds might be recommended to evaluate your baby’s growth and plan for your delivery. Finally, now that you know the consequences of being obese, you can choose to prevent this by scheduling an appointment with doctor Akoury to help you lose professionally before getting pregnant.
Motherhood obesity and overweight: Emotional worries of pregnant women
http://www.awaremednetwork.com/