Gut Neurotransmitters Connection and Addiction
Gut Neurotransmitters Connection and Addiction
With current and ongoing advancements in genetic testing and scientific knowledge, mankind is discovering more about the inner workings of the human body than ever before. Among the new discoveries and paths of inquiry is the link between gut health and psychological and neurological responses. It has been found that gut flora can have a significant influence on the developing brain chemistry of children, which can have an impact on their behavior as adults.
At the Integrative Addiction Conference 2016, experts on the subjects of addiction and nutrition address the link between gut flora, neurotransmitters, and addiction.
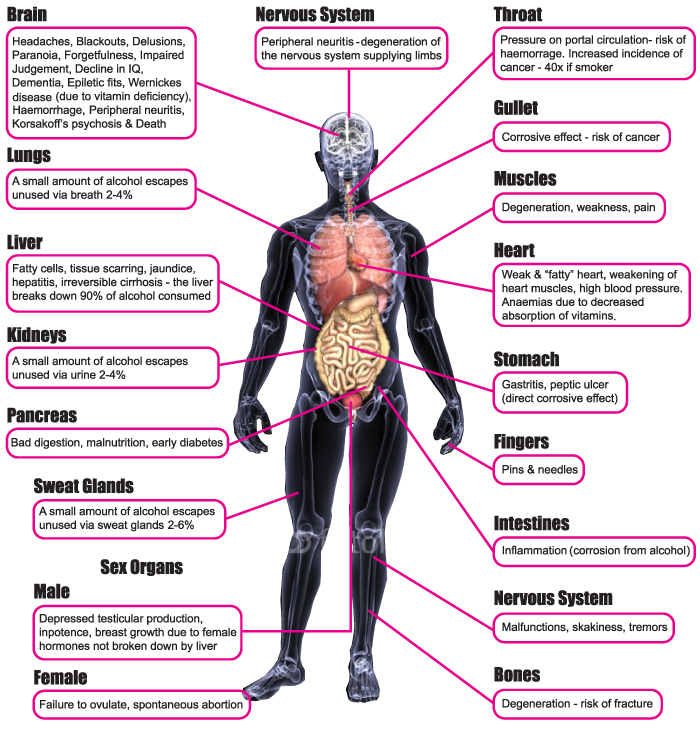
There are over three million bacterial cells inhabiting our bodies, and these bacteria can affect our bodies and minds in ways that we are only just beginning to explore. These bacteria can alter our ability to absorb certain vitamins and other vital nutrients, such as Vitamin B6, which is supposed to promote the health of nerve and muscle cells. Bacteria also affect the body’s immune response, increasing the risk of autoimmune diseases and other illnesses.
 However, the body requires certain beneficial bacteria to function correctly. Strains of Bifidobacterium and Lactobacillus have been shown to not only control numbers of pathogenic bacteria, but also to favorably interact with the immune system and endocrinal system with long-term benefits.
However, the body requires certain beneficial bacteria to function correctly. Strains of Bifidobacterium and Lactobacillus have been shown to not only control numbers of pathogenic bacteria, but also to favorably interact with the immune system and endocrinal system with long-term benefits.
Bacteria and other microbes have also been proven to affect brain chemistry and neurotransmitter production and reception. Studies in rats and mice have shown that those without the beneficial bacteria in their guts have impaired production of Brain-derived Neurotrophic Factor or BDNF. This protein is known to be involved in anxiety response in humans, and low levels have been implicated in various psychiatric diseases including depression and chronic anxiety.
The animals which had no beneficial gut flora also displayed changes in the NMDA and 5HT1A neurotransmitter receptors, which are also involved in mood regulation. In schizophrenia and bi-polar disorder, it is known that part of the cause is a faulty NMDA receptor. Production of tryptophan, the precursor to the generation of serotonin, is also adversely affected by the lack of beneficial gut flora.
Serotonin is a neurotransmitter which regulates our moods. It is also known as the “happiness molecule” and a deficit in serotonin levels is linked to depression, obsessive-compulsive disorder, anxiety, eating disorders, and insomnia, among others. In men, low serotonin levels are expressed as ADHD, impulsive behavior, and excessive drinking. Women are more likely to experience mood imbalances and food cravings.
Dopamine production and reception are also affected by the imbalance of gut flora. Dopamine is the “motivation molecule” and this is what gives us the ability to see things through, as well as giving us a sense of accomplishment when we achieve our goals. Dopamine deficiency manifests as apathy and lack of motivation, lack of ability to experience pleasure, and low libido. Very often the response to low dopamine levels is over-indulgence in pleasure-inducing substances such as alcohol and recreational drugs, or other self-destructive behaviors.
To function properly and be content, the levels of serotonin and dopamine should remain balanced. If we have too much serotonin and not enough dopamine, we feel unable to do anything and lack energy and drive. If dopamine is dominant over serotonin, we are unable to feel happiness and can only see problems without solutions.
 If both dopamine and serotonin levels are low, we will have no motivation and no pleasure or contentment, resulting in depression and cravings.
If both dopamine and serotonin levels are low, we will have no motivation and no pleasure or contentment, resulting in depression and cravings.
Check out our Integrative Addiction Conference 2016 being held in Austin, Texas
A large proportion of these neurochemicals is produced in the gut and affect appetite. It is only recently that research has been made into the possibility that the microbes in the gut produce the substances. As the production of these neurotransmitters and the anatomy of their receptors becomes affected or damaged by the presence of harmful microbes and the lack of beneficial bacteria in the gut, the symptoms associated with their deficiency or imbalance increase. Sufferers rely on ever-increasing quantities of mood-altering substances to balance the shortfall. But the pleasure granted by these devices and substances becomes more and more fleeting, so more and more has to be taken for the same “high”. Thus, addiction is born.
Colonizing the gut with healthy and beneficial bacteria is a process that has to start in childhood to be fully effective in regulating and maintaining brain chemistry. Once the neurotransmitters have been affected, it is much more difficult to rectify the problem and restore the balance. Understanding the problem informs the solution. Adopt a diet that limits gut damage and prevents the release of harmful bacteria into the blood stream. Nutritional supplements and probiotics can restore the beneficial gut flora to healthy levels. There are also supplements that can increase the production and supply of the neurotransmitters. A holistic and integrated approach to a solution will be more effective than treating only the neurochemical imbalance without addressing the cause, which lies in the gut and the gut flora.
The link between the gut, the brain, and addiction will be explored more fully at the Integrative Addiction Conference in August 2016. For more information and to register, visit the website at http://regenerativepotential.com/integrativeaddictionconference/.



 There are a number of ways to potentially treat behavioral addictions. Some approaches may look to study extensively the genetics of the person and then decide the best approach to treatment that way. Others may focus on sociological and/or psychological factors. In essence, the distinction being made here is that of nature versus nurture. However, much like the great philosopher Aristotle said, the best approach to a person’s behavior would be one that understands thoroughly not one or the other, but rather, both of the areas. It is not nature or nurture – it is nature and nurture. The true cultivation of a human being and their habits is derived from both the people we were born as, as well as from the things we learn and the habits we acquire from our teachers and peers. These are simplifications alluding to the age old anthropological debate, but this should be understood as a mere analogy. An integrative approach to behavioral addiction then, is one that takes in to consideration both genetic or neurological data while also considering an individual’s unique social and psychological environment.
There are a number of ways to potentially treat behavioral addictions. Some approaches may look to study extensively the genetics of the person and then decide the best approach to treatment that way. Others may focus on sociological and/or psychological factors. In essence, the distinction being made here is that of nature versus nurture. However, much like the great philosopher Aristotle said, the best approach to a person’s behavior would be one that understands thoroughly not one or the other, but rather, both of the areas. It is not nature or nurture – it is nature and nurture. The true cultivation of a human being and their habits is derived from both the people we were born as, as well as from the things we learn and the habits we acquire from our teachers and peers. These are simplifications alluding to the age old anthropological debate, but this should be understood as a mere analogy. An integrative approach to behavioral addiction then, is one that takes in to consideration both genetic or neurological data while also considering an individual’s unique social and psychological environment.
 The microbiome of our bodies comprises more than 90% of the genetic material present. A study of these organisms and the effect that they have on our body chemistry and processes is a relatively new branch of research, and much of the interactions that govern their behavior and the impact that they have on our physiology are still unknown.
The microbiome of our bodies comprises more than 90% of the genetic material present. A study of these organisms and the effect that they have on our body chemistry and processes is a relatively new branch of research, and much of the interactions that govern their behavior and the impact that they have on our physiology are still unknown. Cravings and addictions can be the body’s way to express deficiencies in certain essential chemicals, such as dopamine or serotonin. A common side effect of dopamine imbalance is an addictive behavior. The person suffering from a shortage of these chemicals will try to find the reactions they create from external sources such as food, alcohol, or drugs. As the addictive substance further impedes the production of the necessary neurotransmitters, more and more is required to maintain the same level of reaction and response. The microbes in the gut also affect anxiety levels, which means that a person with a compromised gut will have a greater level of anxiety and depression, leading to a higher chance of dependence on and addiction to drugs and other mood-altering substances. Unless the root problem of the compromised digestive microbiota is addressed, there is also a greater likelihood that addicts will relapse after rehab, as a result of these elevated anxiety levels.
Cravings and addictions can be the body’s way to express deficiencies in certain essential chemicals, such as dopamine or serotonin. A common side effect of dopamine imbalance is an addictive behavior. The person suffering from a shortage of these chemicals will try to find the reactions they create from external sources such as food, alcohol, or drugs. As the addictive substance further impedes the production of the necessary neurotransmitters, more and more is required to maintain the same level of reaction and response. The microbes in the gut also affect anxiety levels, which means that a person with a compromised gut will have a greater level of anxiety and depression, leading to a higher chance of dependence on and addiction to drugs and other mood-altering substances. Unless the root problem of the compromised digestive microbiota is addressed, there is also a greater likelihood that addicts will relapse after rehab, as a result of these elevated anxiety levels.

