Gut Inflammation Could Be the Source of Your Mood Disorders
As much as this may be shocking to some, it’s a proven medical fact that we all have to believe. There’s now a strong evidence showing the connection between our gut health, brain function and eventually our moods.
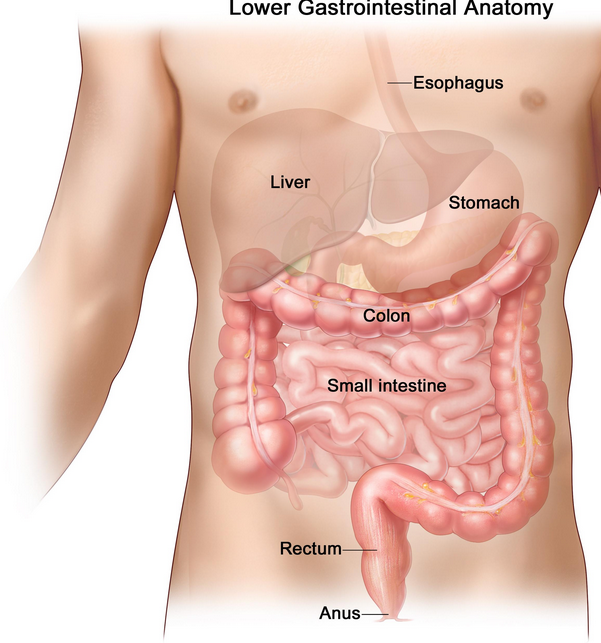
Like most people, I always believed that it’s only stress that can inflict much havoc with our digestive tract. However, as I later found out, problems in our gastrointestinal tract (commonly known as the GI tract) also stand a high chance of negatively impacting our brains and thus causing a lot of anxiety and depression.
Simply put, whatever goes on in your digestive tract has a lot of influence in the CNS-Central Nervous System, your neural circuitry and consequently stands a chance to influence on your behavior- which can be a positive or negative influence.
As revealed in the latest research, there’s for example, a link between how your digestive tract develops in the first few years of one’s life and his or her brain’s health. Subsequently, the influence can be seen later on in his or her future behaviors. The explanation for this hypothesis is based on the fact that a healthy gastrointestinal floral populace impacts positively on the neurons that are tasked with motor control and behavior. In fact, the research concludes that those with distinctly overwhelming population of these gut pathogens (or gut dysbiosis) stand a great chance to develop anxiety and depression in their later lives.
Gut Inflammation and Mood Disorders
For deteriorating gut and intestinal health, a mechanism for the development of systemic inflammation and autoimmunity develops. This is a risky situation given the fact that both conditions of inflammation and autoimmunity have for long been linked with the birth of mood disorders.
As demonstrated in a different research, animal experiments in regards to inflammatory bowel disease proved that this disease had a strong adverse effect on the hypothalamus where it increases the sensitivity of the Hypothalamic Pituitary Adrenal Axis– the HPA, to stress. With all these, it’s only reasonable to affirm the intimate relationship that exist between brain function, gut health and mental health.
According another study on the inflammatory process and depression, addressing inflammation concerns in women who just had their first birth could go a long way in lowering or even prevent the harsh symptoms of post-delivery depression. The research also claims of a cause and effect relationship that exist between Intestinal permeability/GI inflammation and the pathogenesis of alcoholism.
It’s now quite an irrefutable fact that our microbial symbiotic gut inhabitants and ourselves-for which I mean the central nervous system, are in a constant communication through the GABA receptors present in the vagus nerve.
Could Chronic Inflammation result in Depression?
Research has shown that depression could be as a result of gastrointestinal inflammation. The research provides several in attesting to this as below:
- It’s a common knowledge that depressions are in most cases found alongside autoimmune diseases and gastrointestinal inflammations as well as with cardiovascular and neurodegenerative diseases, cancer and type-2-diabetes, all of which chronic low-grade inflammation is a noticeable contributing factor. As a conclusion, the researchers suggested that there’s a likelihood that depression is “neuropsychiatric manifestation of a chronic inflammatory syndrome”
- A dysfunction in the “gut-brain axis” is possibly the primary cause of inflammation as suggested by researchers. According to the researchers and other experts consulted during the research, the gut is literally a second brain- the same identical tissues making the brain during gestation, are the same found in the gut. The gut also has a large amount of serotonin neurotransmitter which plays a big role in mood control
- A good number of clinical studies conducted over time have shown that treatment of gastrointestinal inflammation by use of probiotics, vitamin D and B, and omega-3 fats could worsen the quality of life as well as depression symptoms by offsetting proinflammatory stimuli to the brain.
Free Advice: It’s of great help to understand that the bacteria in your gut form an active and integrated part of your body which essentially, heavily depend on the diet you use and are thus hugely affected by the lifestyle you lead. Too much processed foods and / or sweetened drinks impact negatively on the healthy microflora reducing their population. Sugars in general feed the bad bacteria in the gut and increase their population goes high and the end, systemic inflammation is promoted. Consequently, mood disorders creep in.
Probiotics and Their role in mood disorder
Going a step further in this discussion, could it be possible certain human strains of probiotics cause a therapeutic effect on mood? And could this further emphasize the relationship between gut inflammation and mood disorders? Through several studies conducted, this is factually true.
A particular strain known as the Bifidobacterium infantis, has been shown to considerably influence the stress response by standardizing specific measurements of the Hypothalamic Pituitary Adrenal Axis in addition to immune response and modulation of cytokine, all in an amazing model of depression and stress.
Evidence continue streaming in through research work to support the claim that the brain- our body organ with the sole responsibility of regulating the GI’s functioning through the vagus nerve, is able to communicate directly with the various microbial that form the natural surroundings of the GI tract. In fact, one of the researches conducted claims, “Since the interactions of microbes with host leads to a complex balance of host genes, alteration of microbiota population can cause several metabolic disorders.”

What all these shows is that there is a need to maintain the health of the digestive system’s bacterial interaction (environment) and check the use of probiotics
Maintaining an optimally functioning GI tract is of great significance given the profound prospect of the close relationship and communication between our brain and our gut. Also, this statement should open our eyes to give priority to the GI system when evaluating new patients, lest we wave away from the possible understanding of the causes of many chronic diseases.
AwareMed Wellness and Resource Center
An institution set up to create awareness on healthy living, lifestyle, treatment options on commonly occurring diseases like cancer, addictions etc. We share information on common medical conditions as well as offer accurate treatment to on health problems. Call us or contact us directly from here.
Gut Inflammation Could Be the Source of Your Mood Disorders








Had been treated by severial doctors for depression , bypolar disorder, fibromialga etc. taking large amounts of prescribed drugs with no relief . From antidepressants to pain killers . Had to wing myself of of all meds. do to a bloodclot in my lung which I believe to have been caused by all the prescribed drugs I was taking ( every one of them listed that as a posible side effect ) health cotinued to decline and with only being given more drugs to take which only seemed to numb the pain mentally and physically I stopped taking the prescribed meds and started taking it on myself to live healther ,I have’t had any pain or moodswings which is what lead me to seek a doctors help in the first place. I wasn’t a heavy drinker ,no unprescribed drugs of any kind 25 years in military and could not understand where this was coming from. I’m better now but spend a lot of time worried the pain, depression or both will return.
Great! keep on this great lifestyle changes, pad yourself on the back. Keep reading our blog. and please do not hesitate to seek us if you ever need further help. Great and continuous recovery!!