Stopping brain damage from addiction consequences
Stopping brain damage from addiction consequences is very essential for good health
Stopping brain damage from addiction consequences: The pathological activity
Did you know that drugs are the major cause of the death of the brain cells? The brain is one of the most sensitive organs in any human body where everything starts and ends. Death is always registered the moment ones brain stops functioning. Therefore we all have a duty of keeping the good health of the brain primarily by stopping brain damage from the consequences of drug abuse. To do this, we are going to be consulting with doctor Dalal Akoury MD, to help us in the unlocking some of the sensitive things that we must do to keep the proper functionality of the brain. And in line with that, experts at AWAREmed Health and Wellness Resource Center under the able leadership of doctor Dalal Akoury, are registering that, drug abuse could be the worst cause of damage to the brain.
Stopping brain damage from addiction consequences: Prognosis of recovery
As we progress into the discussion, it is worth noting that the degree of the brain damage from drug abuse is always defined by the prognosis of recovery. Sometimes unfavorable changes in the brain of a drug addict are so much overwhelming that they are not even able to realize the problem let alone the need for treatment. And even if they are, the deformed psyche, expressed in loss of willpower, doesn’t allow them to complete the treatment and refrain from using the drugs. Nonetheless such situations often come to the extreme cases. Besides that under normal circumstances addiction often creates a center of addiction in the brain, or so-called a generator of pathological activity for drug craving.
To illustrate this, let us take an example of a condition we are all familiar with that of epilepsy. This disease is characterized by periodically recurrent seizure syndrome and when a small portion of the brain cells (it can be quite small in size), figuratively speaking, “going crazy”. From time to time they reach the level of excitation which covers the whole brain. As a result, a person loses consciousness, falls down, the total muscle spasms make him convulse. When he comes regains his consciousness, he doesn’t remember what happened to him. Medically these “haywire” cells are called the generator of pathological activity. Now the connection is that about the same generator is formed in case of a drug addiction. However in this case the generator is that of attraction to drugs, self-excitation of which with different periodicity may also cover the entire brain and cause an uncontrollable, overpowering desire to take drugs thereafter. The activity of the generator leads to a constant, obsessive thoughts about drugs. Without treatment, this generator can persist for years, even if the person does not use the drugs during that time. Along with the formation of the generator of attraction to drugs, there is another type of brain damage from drug abuse, to the nervous system of a drug addict.
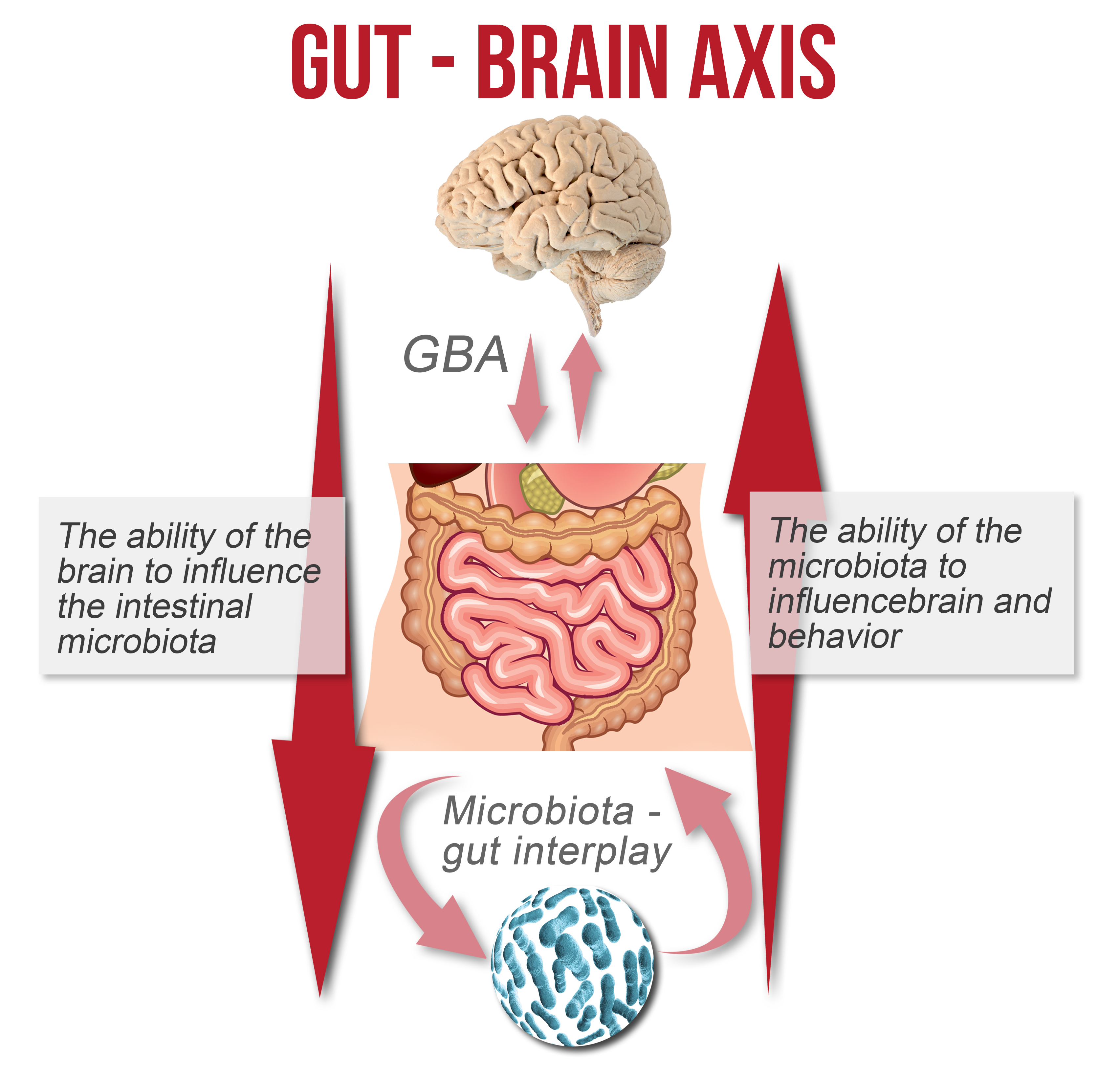
Another reason why stopping brain damage from drug abuse is necessary is because the regular drug poisoning leads to severe changes in metabolism in the cells of the nervous system and especially in brain cells. These cells contain neurotransmitters which are the active substances whose presence in the inter-neuron synapses provides the transmission of electrical impulses to effectuate the functions of all kinds of nervous activities, including the higher nervous activity of a man’s mind, emotions, feelings, willpower, and so on. Doctor Akoury reiterates that the constant presence of the outer psycho active chemical substances badly affects the processes of neuro-transmission in the brain. .
It’s fair to say, that shortly after the “fix”, the deficit of neurotransmitters in an addict’s brain temporarily shifts back to “normal”, and the victim feels better for a while. However, with each subsequent dose of narcotic, the further infringements in neurotransmitter systems of the brain ultimately become more and more profound.
Stopping brain damage from addiction consequences: The pathological activity
http://www.awaremednetwork.com/