Life intimidating diseases related to obesity
Life intimidating diseases related to obesity can occur at any stage of life
Life intimidating diseases related to obesity: Gallbladder disease
Obesity is a major risk factor for gallstones. Being one of the life intimidating diseases, it reduces the number of bile salts in bile, resulting in more cholesterol. Experts at AWAREmed health and wellness resource center under the leadership of doctor Akoury agrees that, emptying gallbladder decreases as a result of obesity
Interventions to obesity: It is the duty of healthcare providers like nurses to help to edge obese people to adopt changes to promote a healthier lifestyle with the main objective being the sustainability of life changes through modification of diet, physical activities and use of community supports.
Life intimidating diseases related to obesity: Safe weight loss approaches
- Widowhood, loneliness, isolation, and depression are other factors that need to be addressed during weight-loss programs.
- The benefits and risks of weight reduction in older adults should be carefully considered.
- Participation in these programs by family members, as well as a caregiver(s), is especially important if the older person’s vision and hearing are impaired or if there is cognitive impairment.
- Older persons present special challenges when making changes in diet and activity levels. In patients over 65, the increase in chronic diseases associated with aging reduces physical activity and exercise capacity, making it more difficult for elderly persons to lose weight.
- Loss of lean body mass, which is already diminished in older adults, may not be appropriate in persons over 65 years of age because the loss of fat-free mass in older adults is associated with significant morbidity and mortality.
- Increasing flexibility, endurance, and strength should be the objective of regular exercise in older adults who are obese.
- Improving physical function and helping to preserve muscle and bone mass through regular physical exercise is important for older adults who are obese.
- Appropriate nutritional counseling through referral to a registered dietitian is necessary to ensure that the older adult’s daily nutritional requirements are met during weight-loss programs.
- A weight loss program that minimizes muscle and bone loss is necessary for the older adults who are obese and have functional impairments or metabolic complications that might be improved by weight loss.
Finally, in ensuring that the life of our old people is well cared for, we must all be involved. To this effect doctor, Akoury made a passionate decision of creating this medical center whose primary objective is transforming each individual’s life through increasing awareness about health and wellness and by empowering individuals to find their own inner healing power. It will further interest you to note that, doctor Akoury’s practice focuses on personalized medicine through healthy lifestyle choices that deal with primary prevention and underlying causes instead of patching up symptoms. This makes her the best option for all your weight management needs. You can schedule an appointment with her on telephone number 843 213 1480 for the commencement of your weight loss recovery program.
Life intimidating diseases related to obesity: Gallbladder disease
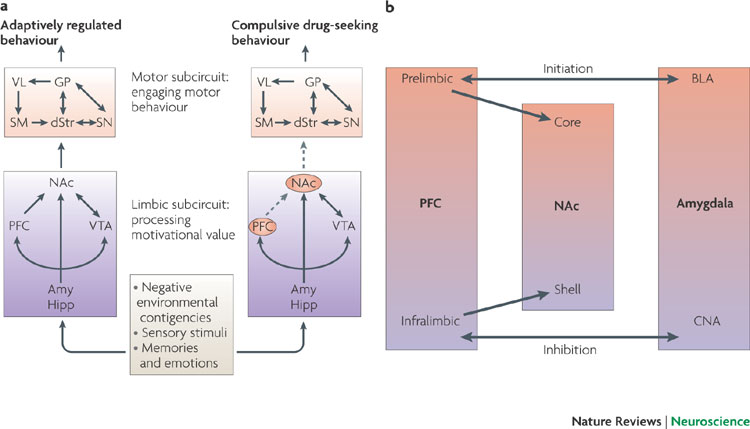
http://www.integrativeaddictionconference.com/wp-admin