Resisting insulin awash in a pool of sugar
Resisting insulin awash in a pool of sugar: Too much insulin

Sugar is a serious drug that is very addictive. Insulin resistance should be a daily practice meaning that we defeat sugar addiction by resisting insulin naturally.
From our previous article we listed too much insulin, cortisol and adrenaline, imbalances of sex hormones like estrogen and testosterone and insufficient thyroid hormones as being epidemic, we now want to look at each in details for a better understanding of the best action to take should you find yourself in situations like this. To start us off into this discussion, we spoke with experts from AWAREmed Health and Wellness Resource Center, a facility that is rich in expertise and very resourceful in terms of addiction health related complications to help us put to perspective what happen when there is too much insulin in the body and how best insulin resistance can be practiced in a day to day way of life. Doctor Dalal Akoury who is the founder of this facility is going to share with us some of the practical examples to help us understand better the magnitude of the problem. This is one piece of information you don’t want to miss and therefore we invite you to stay with us and invite a friend so that together we can make a difference in our societies and defeat all complications that comes with insulin resistance or as we have baptized it resisting insulin.
A few years ago a client I will call Larry (not his real name) came to my office and his story was very interesting and I am persuaded to share with you because I believe it will help you understand the problem from the practical angle. Larry was in his early 40s an executive officer in a reputable organization. He came to me for a cardiac stress test. In his mind he knew that he was dying of heart disease and convincing him otherwise was not very easy. He explained to me how he was feeling and using his own words he said that every afternoon, he would experience sudden onset of sweating, a racing heart, anxiety and shortness of breath. With these signs Larry was convinced that he was dying of heart condition. Besides these he was also stocking some weight around the abdomen.
After listening to him narrate his story, I responded to him in a way that he felt was irrelevant by telling him that “he is not taking his breakfast meals” I also told him that “each time he is eating he feels tired and because of that he often skip meals during the day and that his reason of doing so is to remain alert and focus to his work. My provoking statements did not end there and I continued to tell him that each time he experiences such feelings he often go to the vending machine for a glass of soda to get a quick sugar fix, and that in just a few minutes he feels better and that has become his routine and way of life. In disbelief Larry looked at me shocked, wondering how a total stranger could tell his exactly how he lived his life without him disclosing.
I don’t know if this is communicating to you anything, but I explained to Larry that he was fighting with his genes and was insulin resistant or simply he was resisting insulin leading to wide swings in blood sugar that were responsible for his symptoms. Larry could not regulate his blood sugar because he was pumping out too much insulin and that is how his symptoms became easy to identify. Feeding on too much sugary food stuff like flour, and white rice, your insulin levels spike. This then causes your cells to become resistant to its effects and the consequence of that is that you will pump out more insulin, become more resistant to the ultimate effects and the vicious cycle of insulin resistance continues.
Resisting insulin awash in a pool of sugar: Energy and mood swings
From the story of Larry you realize that to a greater extent, we are the real cause of our insulin problems. While Larry suspicion may have not been accurate, but one point is very clear that insulin resistance has high potential of causing energy and mood swings. According to the experts at AWAREmed Health and Wellness Resource Center, this can come with serious health complications like high blood pressure, heart disease, obesity, cancer, brain aging, dementia, and the list is endless. Another point of concern is that Larry is not alone in this problem of blood sugar control. Available statistics indicate that between 80 and 100 million people in America alone are suffering from insulin resistance. It therefore means that as this practice continues (resisting insulin) each person needs to reevaluate him/herself to be sure and avoid surprises. You can use this formula to test if you are a potential candidate. It has been established that majority of people with insulin resistance have extra fat around the middle. Therefore check your waist-to-hip ratio and the measurement around your belly button. What you get divide by the measurement around your hips. If the solution is greater than 0.8, the chances are that you have insulin resistance. Remember that this is practical irrespective of how you look like. Like for instance, you may be tall, thin, short, fat, or any combination of these and still have insulin resistance. It therefore means that the only way to know for sure is to take an insulin response test, which measures blood sugar and insulin while you are fasting and 1 and 2 hours after you consume a 75-gram sugar drink.
Resisting insulin awash in a pool of sugar: The harmful effect of sugar on our health
Having appreciated how insulin can cause energy and moods swing, let us now interrogate further the other harmful effects of sugar in our health as we come to the end of this section of discussion. The body normally produces insulin in response to food in our stomachs and in particular sugar. When we eat too much sugar we produce insulin in excess and this can result into a variety of health problems as already mentioned above. New findings are establishing that we were not accurate initially when we bought the thought that insulin’s only helps the flow of sugar into cells for purposes of metabolizing and transforming the stored energy of the sun (in plant foods) with the oxygen we breathe into the energy we use every day to run our bodies. New findings reveal many other functions of insulin that affects the body. Ideally when there is too much insulin, the results can be catastrophic and the following are some of the new findings:
- Now we recognize insulin as a major switching station, or control hormone, for many processes. It is a major storage hormone fat storage, that is.
- Insulin acts on your brain to increase appetite, specifically an appetite for sugar. Try as you might, as long as your insulin levels are high you will fight a losing battle for weight loss.
- It increases LDL cholesterol, lowers HDL cholesterol, raises triglycerides, and increases your blood pressure. Insulin resistance causes 50% of all reported cases of high blood pressure.
- It makes your blood sticky and more likely to clot, leading to heart attacks and strokes.
- It stimulates the growth of cancer cells.
- It increases inflammation and oxidative stress and ages your brain.
- It even increases homocysteine because sugar consumption decreases vitamin B6 and folic acid.
- Insulin also causes sex hormone problems and can lead to infertility, hair growth where you don’t want to grow it, hair loss where you don’t want to lose it, acne, low testosterone in men, and more. It also leads to mood disturbances.
Finally it is important to note that insulin resistance is not a genetic defect, an error in our evolution, or a mistake by God. It is just as a result of the simple fact that we have strayed from eating in harmony with our genes. In other words, we do not fit into our genes and you can consult with doctor Akoury for more insight on any concern you may be having.
Resisting insulin awash in a pool of sugar: Too much insulin

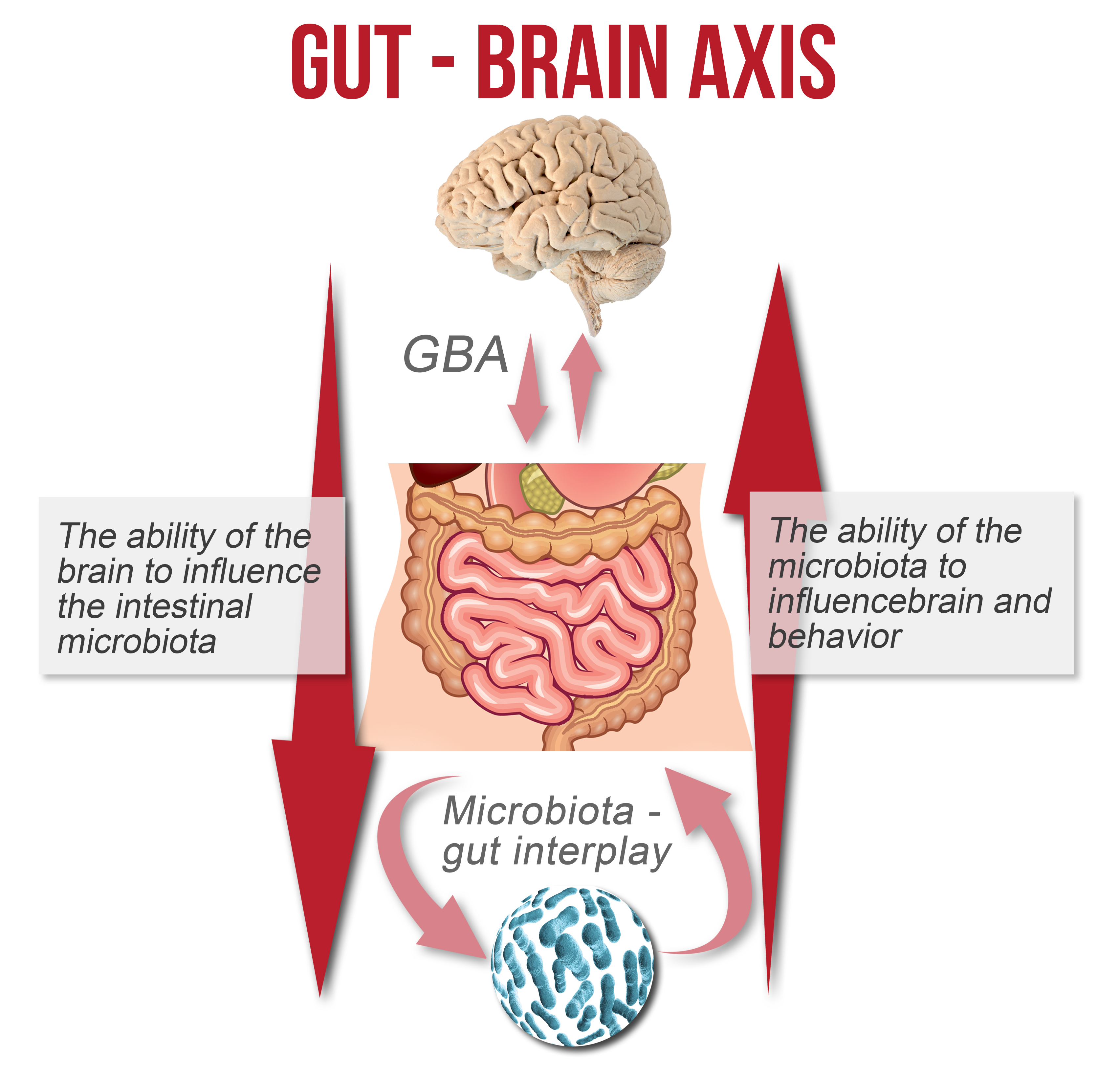
 Although gut-brain health is not a new concept, the depth of the effect of this relationship still does not appear to be particularly widely known at some levels of medicine. With the gut behaving as a second brain and having more neurons than the spine or nervous system, perhaps it is time for the medical profession to take the gut-brain relationship far more seriously in the treatment of physical and mental disease.
Although gut-brain health is not a new concept, the depth of the effect of this relationship still does not appear to be particularly widely known at some levels of medicine. With the gut behaving as a second brain and having more neurons than the spine or nervous system, perhaps it is time for the medical profession to take the gut-brain relationship far more seriously in the treatment of physical and mental disease. Irritable bowel syndrome (IBS) and type II diabetes have also been linked to the gut, with depression and anxiety being caused by an imbalance of intestinal bacteria, rather than the other way around. Many studies are currently underway linking behavior,
Irritable bowel syndrome (IBS) and type II diabetes have also been linked to the gut, with depression and anxiety being caused by an imbalance of intestinal bacteria, rather than the other way around. Many studies are currently underway linking behavior, 
 The microbiome of our bodies comprises more than 90% of the genetic material present. A study of these organisms and the effect that they have on our body chemistry and processes is a relatively new branch of research, and much of the interactions that govern their behavior and the impact that they have on our physiology are still unknown.
The microbiome of our bodies comprises more than 90% of the genetic material present. A study of these organisms and the effect that they have on our body chemistry and processes is a relatively new branch of research, and much of the interactions that govern their behavior and the impact that they have on our physiology are still unknown. Cravings and addictions can be the body’s way to express deficiencies in certain essential chemicals, such as dopamine or serotonin. A common side effect of dopamine imbalance is an addictive behavior. The person suffering from a shortage of these chemicals will try to find the reactions they create from external sources such as food, alcohol, or drugs. As the addictive substance further impedes the production of the necessary neurotransmitters, more and more is required to maintain the same level of reaction and response. The microbes in the gut also affect anxiety levels, which means that a person with a compromised gut will have a greater level of anxiety and depression, leading to a higher chance of dependence on and addiction to drugs and other mood-altering substances. Unless the root problem of the compromised digestive microbiota is addressed, there is also a greater likelihood that addicts will relapse after rehab, as a result of these elevated anxiety levels.
Cravings and addictions can be the body’s way to express deficiencies in certain essential chemicals, such as dopamine or serotonin. A common side effect of dopamine imbalance is an addictive behavior. The person suffering from a shortage of these chemicals will try to find the reactions they create from external sources such as food, alcohol, or drugs. As the addictive substance further impedes the production of the necessary neurotransmitters, more and more is required to maintain the same level of reaction and response. The microbes in the gut also affect anxiety levels, which means that a person with a compromised gut will have a greater level of anxiety and depression, leading to a higher chance of dependence on and addiction to drugs and other mood-altering substances. Unless the root problem of the compromised digestive microbiota is addressed, there is also a greater likelihood that addicts will relapse after rehab, as a result of these elevated anxiety levels.