Neurochemical basis of addiction

Neurochemical basis of addiction and addiction treatment systems
Neurochemical basis of addiction: The depleted GABA
For a long time, various forms of addictions have been taken to be just as a result of social problems and sometimes even decisions or choices we make in life. Yes, this may be true but we need to take a moment and look into this problem more critically to find facts about the neurochemical basis of addiction. Doctor Dalal Akoury MD, President, and founder of the AWAREmed health and wellness resource center says that it’s good that modern addiction medicine now recognizes that substance dependency of any kind is a disease process of the brain that features lowered dopamine and glutamate neurotransmitter levels. Importantly, as more legitimate research is done in this field of addiction medicine whose experimental basis is beginning to gain ground, models of neurochemical bases of addiction in the future may also feature lowered levels of GABA as the disease progresses. To understand this neurotransmitter (GABA) it will be necessary that we try to define some of the terms associated with it and appreciate the roles and functions of GABA in totality.
Because of our unique DNA and the way that each of us metabolizes drugs, each of us may have different amounts of GABA in the brain but we are still considered to be operating “normally.” Unfortunately, there are no accepted medical tests to determine if we have too much or too little GABA activity. It appears that people who are nutritionally deficit and dehydrated often have problems with the operation of GABA in their brains. Since almost all of our patients are nutritionally deficient and dehydrated when they arrive at our facility, we have always implemented the addition of GABA to the IV therapy given to patients. The purpose is to provide a more natural boost to the GABA in the brain and to allow the calming effect of GABA to make the detoxification process more comfortable. Let us now understand how GABA operates by defining these terms.
Neurochemical basis of addiction: The neuron
- A neuron is another name for a nerve cell.
- Nerve cells float in the fluid.
- Each neuron has an axon a thread-like part of the cell that sends signals from the cell body and a dendrite a part of the cell that receives signals from other neurons.
- The neurons are not touching and the space between the cells is called the synapse.
- Electrical signals are sent through the synapse to a receptor, a place on a cell that can produce a certain effect like the production of adrenaline if someone is frightened.
Neurochemical basis of addiction: The central nervous system (CNS)
- The CNS is composed of the brain and the spinal cord.
- The CNS transmits signals to the rest of the body using chemical messengers called neurotransmitters.
- Neurotransmitters are stored in vesicles—hollow sac-like structures inside the cells.
- These neurotransmitters carry a message from a neuron to receptors on another neuron.
- The action of the neurotransmitters on the receptors has been likened to a key being inserted in a lock.
- When the key is turned the lock opens and the neurotransmitters activate the receptors which in turn create an effect in the body.
- Then many of the neurotransmitters return to the releasing vesicles to be used again.
Finally, you can always talk to us by calling doctor Akoury on telephone number 843 213 1480 to help you with any concerns you may have.
Neurochemical basis of addiction: The depleted GABA
http://regenerativepotential.com/wp-admin




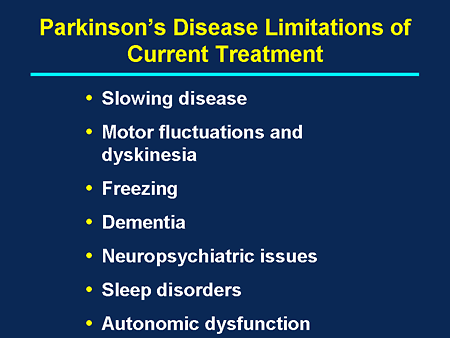 In 1980-90s researchers worked to find out if the cell replacement therapy could be used to quell the harmful effects of the Parkinson’s disease. The findings of these researchers have since been a foundation upon which current researchers increase the scope of their study on the effects of cell replacement therapy on the Parkinson’s disease. Particularly, Swedish, American and Canadian researchers have transplanted the developing nigral dopamine-producing neurons from human fetuses into animals and human patients with Parkinson’s disease. In these studies there were some great improvements while in other cases there were only modest changes.
In 1980-90s researchers worked to find out if the cell replacement therapy could be used to quell the harmful effects of the Parkinson’s disease. The findings of these researchers have since been a foundation upon which current researchers increase the scope of their study on the effects of cell replacement therapy on the Parkinson’s disease. Particularly, Swedish, American and Canadian researchers have transplanted the developing nigral dopamine-producing neurons from human fetuses into animals and human patients with Parkinson’s disease. In these studies there were some great improvements while in other cases there were only modest changes.





 Nicotine and Neurochemicals
Nicotine and Neurochemicals