Good neurotransmitters and moods for addiction healing
Good Neurotransmitters and moods for addiction healing as away of containing substance abuse
Good neurotransmitters and moods for addiction healing: Feeding on good nutrition
In the process of seeking for solutions when it comes to overcoming drug addiction, people often go for very big things, big rehabilitation institutions and expensive and elaborate addiction professionals. I certainly don’t have any problem with that for it is very much in order since the most important thing is the reclaiming of one’s health and freedom from the scourge of addiction. However what many may not know or if they do, then they don’t care about is the avenue of nutrition as a tool of fighting and eliminating all sorts of addictions you may be privy to. For quite a while now we have been posting articles touching on the use of healthy nutrition in the fight against substance abuse and we are not about to stop. We want all of us to have the knowledge so that the work of dealing with drug addiction can be made easier and much lighter to both the direct and indirect victims. From the expert’s point of view, correcting addiction by good neurotransmitters and moods is one very important avenue available for containing the problem.
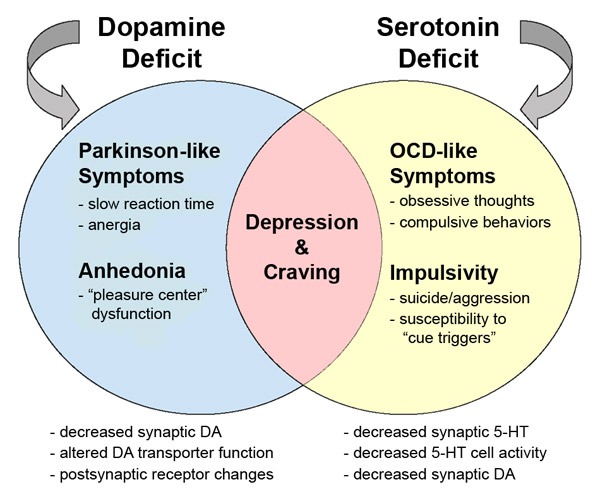
According to doctor Dalal Akoury (MD) a well-respected expert in addiction, it is important to note that psychoactive substances may lead to psychiatric problems because in many cases the substances can have toxic effects on brain chemistry. She adds that before detoxification is done, neurotransmitters are reduced due to poor nutrition which then alters the amino acid absorption and utilization. The implication of this is that the victims (addicts) are left feeling depressed, agitated and unregulated early in recovery. From the various studies conducted so far, it is believed that these imbalances will disappear over a couple of weeks but then again, they may also last as long as one year after an addict becomes sober further necessitating normalizing neurotransmitters and moods for the perfection in addiction healing process.
Good neurotransmitters and moods for addiction healing: Moods and behavior abnormalities
As we progress into the discussion, it is worth noting that for some, moods and behavior abnormalities may have been present before the substance abuse. With proper diagnosis of any possible underlying mental health disorders, a healthy diet and education on how nutrition influences mood and brain chemistry, recovery can be enhanced. An understanding of how food affects mood and the risk of substance abuse begins with macronutrients. And with carbohydrates being the body’s main source of energy it therefore means that without this macronutrient, the brain can’t function properly, blood sugar becomes unstable, and neurotransmitters become disrupted. Unstable blood sugar can lead to feelings of frustration, anxiety, and cravings. You can however avoid this by scheduling for an appointment with doctor Dalal Akoury today for a more professional input that will help you effectively in the normalizing neurotransmitters and moods for addiction healing.
Good neurotransmitters and moods for addiction healing: Feeding on good nutrition
http://www.integrativeaddictionconference.com/wp-admin