Building gut lining for good health
Building gut lining for good health and healthy brain activities that eliminate addiction
Building gut lining for good health: The villi and microvilli
Gut health treatment is done in phases and the second phase involves giving your body what it needs to rebuild the gut lining. Experts from AWAREmed Health and Wellness Resource Center have associated the inside of the small intestine to a towel covered with millions of little loops (called villi), which are further covered with millions of little fibers known as microvilli. If the gut is leaky, those fibers get matted thereby hampering regrowth and the absorption of nutrients from food and the vicious cycle continues because the villi need those nutrients to survive. Therefore to solve this riddle building gut lining for its good health is very important and expert recommends:
Eat whole foods in plenty: The body needs food nutrients in their real, fresh food to repair any damage and rebuild healthy new tissue. Whole foods are full of vitamins, minerals, and phytonutrients, plus enzymes the small intestine needs to heal. You can also prioritize non-starchy vegetables and lean proteins by eating plenty of good, whole-food which help strengthen cellular membranes. Therefore as the body heals, it will trigger the elimination of toxins and other byproducts through the large intestine. And for this to happen, the body will need lots of fiber inform of roughages from the food stuff from colorful vegetables, berries, legumes, nuts, seeds, and whole-kernel grains.
Supplement with glutamine: Glutamine supports immunity and digestion by fueling the cells that line the small intestine. Glutamine heals the intestinal lining more than any other nutrient.
Omega-3 fatty acids: These are beneficial to the gut calming inflammation and rebuilding healthy cell walls.
Building gut lining for good health: Re-inoculate
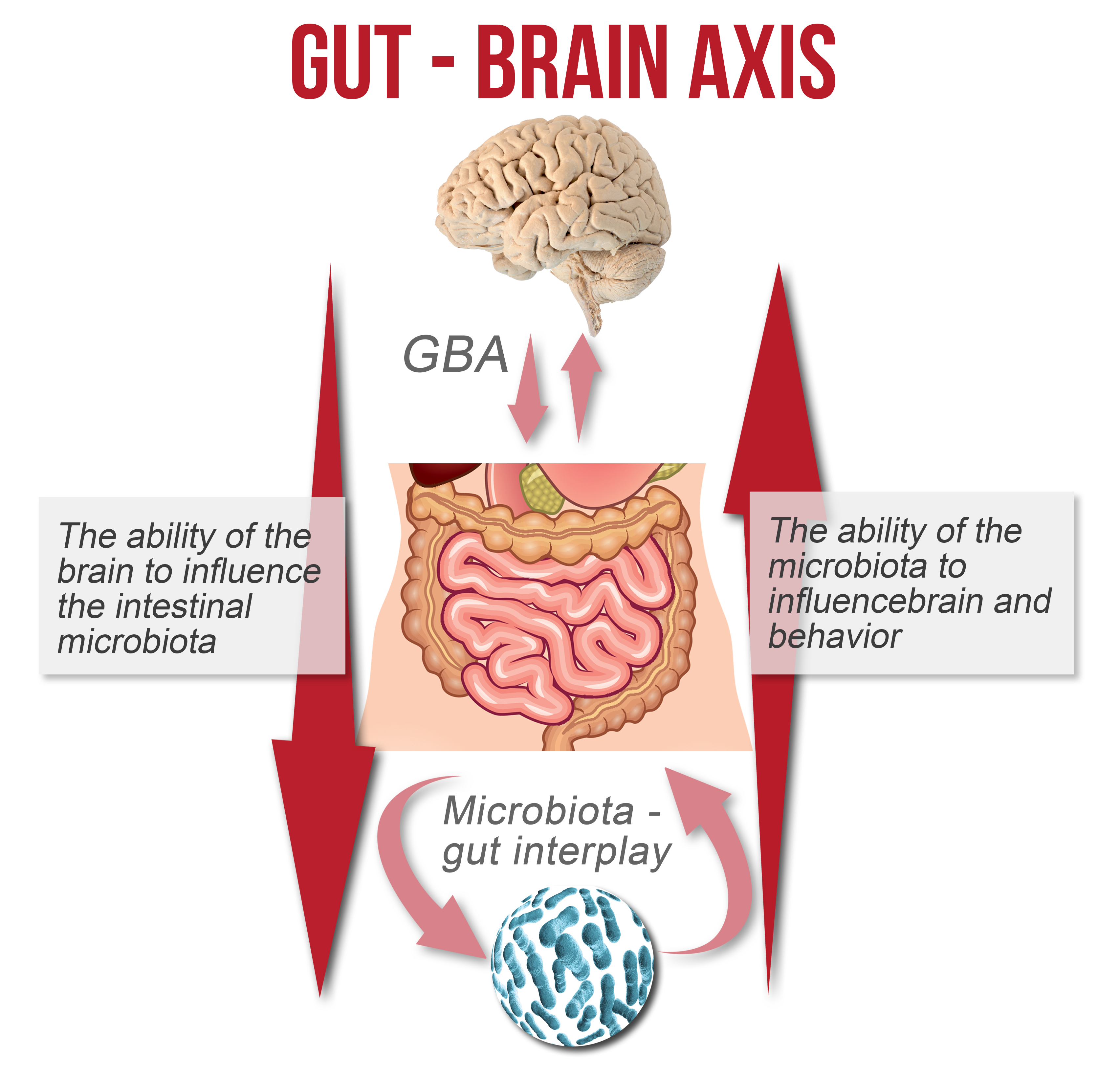
Once your body has patched up the leaks in the gut, you need to help it grow a healthy layer of good bacteria flora that helps protect the GI tract and assist with digestion. These beneficial bacteria strengthen your immune system, improve metabolism, help your body make vitamins, and aid in the absorption of minerals.
Add a probiotic: High-intensity probiotic support rejuvenates and replenishes a microbiome damaged by antibiotics or a poor diet. Doctor Akoury recommends a high-potency probiotic of at least 50 billion active cultures twice daily.
Building gut lining for good health: Repair and rebalance
Finally, once you’ve got your gut on the road to wellness, it’s time to focus on lasting lifestyle changes. Sliding back into the habits that caused your leaky gut will only invite the return of health problems you want to avoid. Here are two key strategies for supporting ongoing gut health:
Eat mindfully: this may sound off the show but nonetheless before taking your first bite, look at your food and take in its aroma. This will trigger the cephalic phase of digestion, an initial release of enzymes that help break down your food. And as you eat, chew thoroughly, paying attention to your food’s flavor and texture. Avoid multitasking or rushing while you eat. Take pauses and breaths between bites, allowing your digestive system to keep pace.
Calm your central nervous system: when stressed, the body’s nervous system kicks into fight-or-flight mode the opposite of rest-and-digest mode. Recalibrate by cultivating a calmer, more centered state. Consider a daily meditation or yoga practice. Or on a stressful day, swap heavy weightlifting for a tai-chi class. Take note that each time when you change your thoughts you change your physiology as well. Call doctor Akoury for more professional input in building gut lining today.
Building gut lining for good health: The villi and microvilli
http://www.integrativeaddictionconference.com/wp-admin