The stress cycle and impact on beauty
The stress cycle and impact on beauty – How Stress Can Wreak Havoc on Your Hair and Skin

The stress cycle and impact on beauty is real since stress also widens blood vessels, which causes redness and aggravates rosacea
It is very ironical that beauty is sort by everyone across the globe yet one of the biggest enemies of beauty is stress which is also a common problem to everybody globally today. While we all want to look radiant composed and beautiful, managing situations which stresses us is an uphill task in our daily lives. In the process of juggling with beauty and stress we find ourselves compromising in most cases and the stress cycle and impact on beauty continuous. To overcome this stress cycle, we need to get the experience opinions of the experts at AWAREmed Health and Wellness Resource Center under the able leadership of Doctor Akoury’s care. Doctor Akoury founded this facility to offer her expertise help to many people who are struggling with the health of their skin. It has been established that stress is one of the major obstacle to attaining optimum beauty and this is what is being addressed professionally at this facility. Therefore for ultimate beauty, you can call doctor Akoury today to schedule for an appointment to commence treatment right away. In the meantime, we want to further look into ways and means through which stress is becoming an impediment of beautiful skin.
There is a lot of science behind the stress and its effects to the skin.
- Actually the way stress affects your skin is that when you’re anxious, your brain releases cortisol, a stress hormone, into your bloodstream.
- This then communicates to the oil glands to ramp up production, leading to breakouts.
- Stress also widens blood vessels, which causes redness and aggravates rosacea.
- Another side effect is that the skin becomes dehydrated, sensitive, and more susceptible to damage.
- Besides causing lines from furrowing your brow, stress also makes you look markedly older.
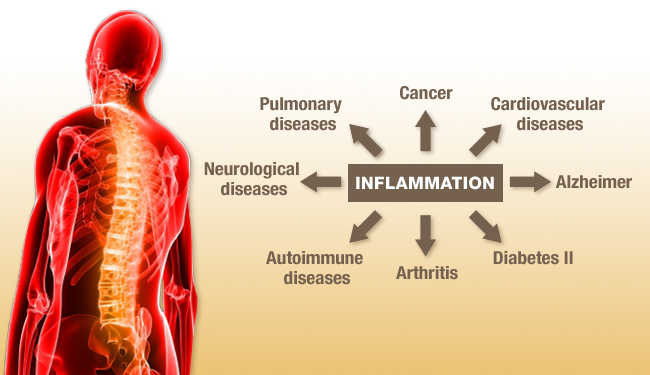
Ordinarily the human body loses one percent of its skin’s collagen supply every year at the age 20, however with stress this can be accelerated further. It is therefore proper to say that majority of younger women are visiting many skin care professionals to have their wrinkles eliminated while much older ones are also struggling with acne. These issues are caused in large part because majority of the people seeking for such treatments are more stressed out than they were even five or a few years ago. Some triggers of stress may include: relationships, money, work, and family among many others. Nonetheless we are also seeing a considerable rise in cultural stress i.e. the feeling that women expect perfection from themselves in all areas at all times. While appreciating that stress is radically unhealthy for your major body organs like the heart and the brain, it is also very important to take note of the damage it causes to the skin which is also the largest organ of the body. The effect of stress on the skin is not something one should take lightly and so we want to look further on the stress cycle and impact on beauty.
The stress cycle and impact on beauty – How Stress affects Your Hair and Skin
Much as we may not agree with it, stress is not just an irritating byproduct of everyday life but it is also a major health and beauty trespasser. A simple lack of sleep, dehydration, and junk food cravings often go hand-in-hand with stress, which trickles down to poor hair and skin health. You’d be surprised to know that stress could actually be the root of these six beauty issues.
It weakens overall skin and hair health – Stress can interrupt sleep patterns a key component for skin and body repair. Coupled with stress, skimping on sleep weakens the immune system and puts the body’s chemicals out of smack, often leaving you with lackluster skin and dull eyes.
It promotes skin irritants – Stress also causes you to release certain hormones, which can trigger your body into channeling blood away from the skin toward muscles and other organs. In particular, chronic stress deprives your skin of oxygen and essential nutrients and without adequate amounts of them you get skin conditions like acne.
It dries out everything – The negative effects of stress can present themselves on the skin with extreme dehydration that results in:
- Inflammation
- Hyperpigmentation
- Dullness and
- Acne
It must be remembered that when the stress cycle and impact on beauty exceeds the limit, the dead cell layer on the surface of the skin becomes thin and develops microscopic holes, which cannot provide sufficient defense against aging and ultraviolet rays. Again not only can stress cause breakouts, but it also creates tiny perforations in cell membranes that allow water to leak from cells and dehydrate the skin. That’s when fine lines and a lackluster skin tone begin to appear.
It gives you wrinkles – Stress hormones increase blood pressure, raise pulse rates and constrict blood vessels, which in turn redirect blood away from the skin towards other organs. The result is that our muscles tense, our skin loses that rosy glow, and wrinkles begin to form.
It causes hair loss – As stress causes the blood vessels to constrict, hair follicles are then deprived of the oxygen, minerals, and vitamins they need for healthy hair growth. Therefore when you’re feeling so frazzled, your body burns more energy and directs the vitamins and nutrients to those body parts that it needs for survival like the heart, lungs, and brain. This would then means that your scalp will not get the benefit of these essential nutrients.
Over the years it has become easy to spot clients who are dealing with a lot of stress. Signs like hair loss, hair thinning, and an overall lack of shine and luster are common. In extreme cases, patients start to suffer from ailments such as Alopecia and Psoriasis, both of which contribute to weak and fragile hair that breaks easily.
It leads to bad beauty habits – Sometimes severe stress can lead to formation of nasty habits like hair twirling or twisting or nail biting which become almost subconscious. All that twisting can result in chronic trauma to the hair in some areas, leading to broken hair and even hair loss.
The stress cycle and impact on beauty – How Stress Can Wreak Havoc on Your Hair and Skin